Moral distress is a threat to nurse retention. It plagues significant numbers of nurses and many other health care professionals. Not being able to fulfill his or her nursing obligations for their patients due to intractable value conflicts, ineffective communication, lack of teamwork, organizational oversights, staffing policies, and pressures on health care systems undermines the integrity and well being of everyone. How can one be a good nurse when he/she is forced to go against their “moral compass” on a regular basis? What then becomes the best possible health care service you can provide to those you serve?
Moral distress is a predictable response to situations where nurses recognize that there is a moral problem, have a responsibility to do something about it, but cannot act in a way that preserves their integrity. Imagine this: You are a nurse on a busy medical-surgical unit. A new patient is admitted with severe abdominal pain; you already have five other sick patients. This new patient does not react well to the pain medication the physician has been giving her and continues to request additional doses because of unrelieved pain. You know the dose is not enough and call the physician, but cannot convince the physician to alter the drug dosage. She states that she’s worried about masking important assessment data and using larger doses of narcotics in light of national concerns about over-prescribing them. While legitimate concerns, you are faced with witnessing the patient’s suffering and not being able to relieve it. You are left to try to reassure the patient, attempt other comfort measures, inform the supervising nurses, go up the medical chain of command, document the situation, and go on to care for you other patients. You wonder, “How can I be a ‘good nurse’?” The feeling of not being able to do the right thing, despite your protests, is called moral distress.
Moral distress has become a leading cause for nurses leaving hospitals, systems, or even the profession itself, which raises the question: how do we effectively address it? Since moral distress traces its roots back to the organization or system itself, establishing a culture of ethical practice must become a bigger priority. But even when a culture of ethical practice is established, moral distress is unlikely to be eliminated. Organizations are comprised of individuals who contribute to the culture. This means that the individuals in organizations must be morally resilient to change the status quo. When individuals have it, the culture can thrive.
Moral resilience begins with cultivating self-regulation and self-awareness to recognize when integrity is threatened. With this foundation, nurses are better able to name the ethical problem, inquire into the facts, and determine action that supports integrity. What is at stake? What can be done? Can there be a compromise? Using tools of ethical reasoning and reflection to identify ways to support both the patient and clinicians can help to build moral resilience.
Not only does teaching moral resilience help the nurse in his/her career, but it encourages lessons that can translate over to everyday life. It teaches self-discipline, how to listen and respect views that are different from your own, not to exert personal agendas, and to be able to articulate a point of view in a coherent, ethically grounded way.
Despite three decades of research documenting the incidence and impact of moral distress, few interventions have been proven to relieve it. Now there is the realization that simultaneous interventions focused on both individuals and organizations will be necessary to turn the destructive tide of moral distress. The recent symposium on transforming moral distress focused on the promising practices to address these gaps. Hospital ethics committees are expanding their services to address the sources of moral distress. Nursing schools are adding more content on ethics and resilience. And there is greater awareness about the link between moral distress and burnout. But, when all is said and done, it starts with the individual nurse and the moral resilience built within.
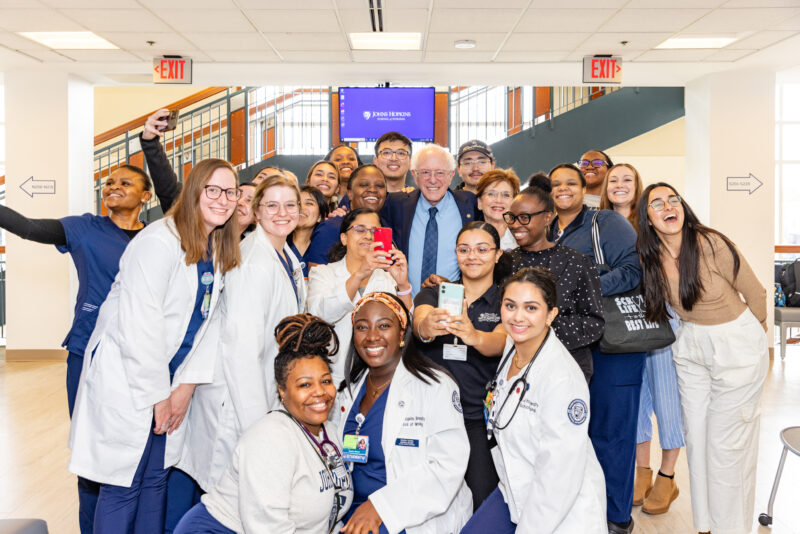
Recently, the American Journal of Nursing published “State of the Science: Transforming Moral Distress into Moral Resilience in Nursing,” a report on the Moral Resilience summit held at the Johns Hopkins School of Nursing, addressing the problem of moral distress and the many ways resilience can be built within the nurse.
ABOUT THE AUTHOR: CYNDA RUSHTON, PhD, RN, FAAN
 Cynda Hylton Rushton is the Anne and George L. Bunting Professor of Clinical Ethics in the Johns Hopkins Berman Institute of Bioethics and the School of Nursing, with a joint appointment in the School of Medicine’s Department of Pediatrics. Her current scholarship in clinical ethics focuses on moral distress and suffering of clinicians, the development of moral resilience, palliative care, and designing a culture of ethical practice.
Cynda Hylton Rushton is the Anne and George L. Bunting Professor of Clinical Ethics in the Johns Hopkins Berman Institute of Bioethics and the School of Nursing, with a joint appointment in the School of Medicine’s Department of Pediatrics. Her current scholarship in clinical ethics focuses on moral distress and suffering of clinicians, the development of moral resilience, palliative care, and designing a culture of ethical practice.